New mRNA-Based Injection Shows Promise in Preventing Preeclampsia, Using COVID Vaccine Technology
The groundbreaking technology behind mRNA COVID-19 vaccines may soon offer a solution to a dangerous pregnancy complication: preeclampsia. A recent study published in Nature highlights the potential of mRNA-based injections to reduce the risk of preeclampsia in lab mice, paving the way for innovative maternal-fetal health interventions.
Preeclampsia, characterized by persistent high blood pressure during or after pregnancy, poses severe risks to both mother and baby, including life-threatening complications and organ damage in the mother. Affecting 3% to 5% of pregnancies, the condition currently lacks a cure. Treatment is limited to managing symptoms through blood pressure medications or bed rest.
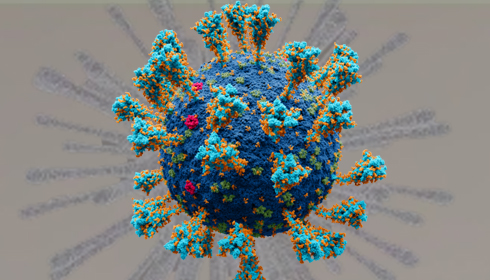
The experimental injection, developed by researchers at the University of Pennsylvania School of Engineering and Applied Science, utilizes lipid nanoparticles (LNPs) to deliver an mRNA therapeutic directly to the placenta. This targeted approach improved blood flow to the placenta, stabilized maternal blood pressure through the end of pregnancy, and enhanced fetal health. The study also reported an increase in litter weight in lab mice, signaling healthier outcomes for both mother and offspring.
Kelsey Swingle, the lead researcher and a doctoral student in bioengineering, explained the innovation: "The injection was able to deliver an mRNA therapeutic that reduced maternal blood pressure through the end of gestation and improved fetal health and blood circulation in the placenta." This method addresses the root cause of preeclampsia—restricted blood flow to the placenta—by using the same delivery system as mRNA COVID-19 vaccines.
To identify the optimal lipid nanoparticle for this application, Swingle screened 98 different formulations, ultimately discovering one that was 100 times more effective in delivering mRNA to the placenta compared to an FDA-approved alternative. A single injection provided sustained relief from preeclampsia symptoms in pregnant mice until the end of their pregnancy.
The next phase of the research will involve testing the injection in larger animal models, such as rats and guinea pigs, whose placental structures more closely resemble those of humans. These studies aim to refine the dosage and evaluate the treatment's efficacy in preparation for eventual human clinical trials.
Beyond preeclampsia, the study underscores the broader potential of lipid nanoparticles in delivering treatments for various diseases and disorders. As Swingle noted, “This research shows the potential for using lipid nanoparticles to deliver cures for other diseases and disorders.”
If successful in further trials, this approach could revolutionize maternal healthcare, offering a lifeline for expectant mothers and their babies while opening new avenues for mRNA-based therapies.