UCLA scientists develop immune cells for ready-to-use cancer immunotherapy
Scientists from California State University, Los Angeles (UCLA) said that they have unveiled a groundbreaking system to wangle immensely potent vulnerable cells with the eventuality of revising "off-the-shelf" cell remedies for gruelling cancers.
In the realm of out-of-stock" cell remedies, also known as allogenic remedies, vulnerable cells sourced from healthy benefactors replace those from cases.
This approach could pave the way for further timely and accessible cell curatives like fantastic antigen receptor(auto) T cell remedies, a monumental vault in prostrating the hurdles that hamper the delivery of life-saving treatments to cases.
Lili Yang, associate professor of microbiology, immunology, and molecular genetics and a member of the UCLA Health Jonsson Comprehensive Cancer Centre, emphasised the urgency of time in treating advanced cancers.
She developed, Currently, these types of curatives need to be acclimatised to the individual case. We've got to prize white blood cells from a case, genetically wangle the cells, and also re-infuse them back into the case. This process can take weeks to months and can bring hundreds of thousands of bones to treat each case."
The new approach, published in Nature Dispatches recently, marks a vital stride towards creating more effective and cost-effective cell curves that can be produced on a mass scale and distributed to hospitals worldwide.
This development has the implicit effect of making auto-T cell remedies not only more affordable but also readily accessible to a broader population.
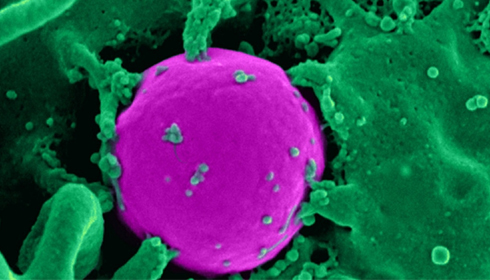
The study conducted by Yang and her platoon zeroed in on gamma delta T cells, a type of vulnerable cell honoured for its capacity to target a variety of cancers, including solid excrescences, all while escaping graft-versus-host complaints, a common complication associated with allogeneic cell curatives.
While gamma delta T cell-based treatments have been explored preliminarily, their clinical success has been limited due to patron variability, short-lived continuity, and the cancer cells' capability to shirk the vulnerable system.
Yet, Yang and her colleagues discovered pivotal advanced gamma delta T cells featuring high expressions of a CD16 face marker that displayed a significantly enhanced capability to combat cancer cells.
Explaining their findings, Yang said," These CD16-high gamma delta T cells parade unique characteristics that increase their capability to fete an excrescence. They demonstrate heightened levels of effector motes and are equipped with the capability to engage in antibody-dependent cellular cytotoxicity against cancer cells. Using CD16 as a biomarker for patron selection significantly enhances their anti-cancer parcels."
Similarly, the experimenters overcame former challenges linked to gamma delta T cell treatments by equipping the cells with Auto and IL-15, the two essential factors that amplify the cancer-fighting prowess of gamma delta T cells.
With this groundbreaking approach, the scientists efficiently produced a large volume of these potently finagled cells, which were later tested on two distinct preclinical ovarian cancer models.
The results were astonishing, as the cells effectively attacked excrescences and remained within the models for extended ages, sustaining their anti-tumour impact.
Remarkably, the research team did not encounter complications similar to those seen among the graft-versus-host complaint.
Commenting about her findings, Yang stated," The results of this exploration shed light on the promising feasibility, remedial eventuality, and remarkable safety profile of these finagled CD16-high gamma delta T cells. We hope this can be a feasible remedial option for cancer treatment in the future."