New HIV Prevention Drug Shows 100% Efficacy in Clinical Trial: A Game Changer for Young Women
A groundbreaking clinical trial in South Africa and Uganda has demonstrated that a twice-yearly injection of a new pre-exposure prophylaxis (PrEP) drug, lenacapavir, offers young women complete protection from HIV infection. This trial, which tested lenacapavir against two existing daily PrEP pills, could revolutionize HIV prevention, particularly among the vulnerable young female population in eastern and southern Africa.
The Purpose 1 trial, involving 5,000 participants at multiple sites in Uganda and South Africa, compared the efficacy of lenacapavir, a six-monthly injectable drug, with two daily PrEP pills: Truvada (F/TDF) and Descovy (F/TAF). The results were striking: none of the 2,134 women receiving lenacapavir contracted HIV, compared to 16 out of 1,068 women on Truvada (1.5%) and 39 out of 2,136 women on Descovy (1.8%).
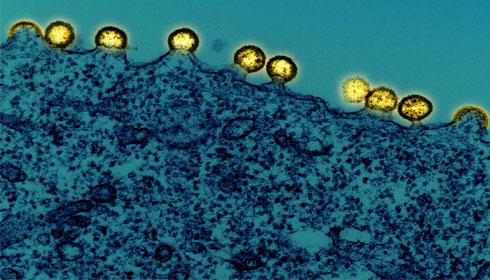
Lenacapavir, a fusion capsid inhibitor, disrupts HIV’s protective shell, preventing the virus from replicating. This novel mechanism, coupled with its long-lasting effect, makes it a promising alternative to daily PrEP regimens, which many young women find challenging to maintain due to social and structural barriers.
The 100% efficacy of lenacapavir in the trial offers substantial hope for reducing new HIV infections. Despite global efforts, 1.3 million new infections were recorded last year, underscoring the need for more effective prevention methods to meet UNAIDS targets and ultimately end AIDS by 2030.
Physician-scientist Linda-Gail Bekker, principal investigator for the South African part of the study, highlighted the potential impact of this drug. "For a young woman who struggles to get to an appointment at a clinic in a town or who can't keep pills without facing stigma or violence, an injection just twice a year is the option that could keep her free of HIV," she explained.
The trial's success led to an independent data safety monitoring board recommending the end of the trial’s blinded phase, allowing all participants to choose their preferred PrEP method. This significant step indicates the high safety and efficacy profile of lenacapavir.
The Purpose 1 trial will now enter an open-label phase, with participants informed of their treatment groups and given a choice of PrEP. Meanwhile, a sister trial, Purpose 2, is underway, testing lenacapavir among cisgender men, transgender, and nonbinary individuals in various regions, including Africa.
The immediate goal is to submit the trial results to regulators in Uganda, South Africa, and potentially other countries. The World Health Organization (WHO) will also review the data and may issue recommendations, paving the way for lenacapavir to be included in global and national HIV prevention guidelines.
However, accessibility and affordability remain crucial challenges. Gilead Sciences, the drug’s developer, plans to offer licenses for generic manufacturing to reduce costs, essential for widespread public sector distribution.
The trial's success marks a significant milestone in HIV prevention, offering a highly effective, long-acting option that could overcome many of the barriers associated with daily PrEP regimens. If implemented widely, lenacapavir could drastically reduce HIV infection rates among young women in high-risk regions, bringing us closer to the goal of ending AIDS by 2030.