MUCORMYCOSIS
Mucormycosis (previously known as zygomycosis), is a serious but rare fungal infection caused by a group of molds called mucormycetes. These fungi can be commonly found in soil and in decaying organic matter, such as leaves, or rotten wood. Mucormycosis largely affects population suffering from other health ailments or taking medicines that lower the body’s ability to fight germs and illness. It most commonly affects the sinuses or the lungs after inhaling fungal spores from the air.
It can also infect oral cavity or brain, gastrointestinal tract and can occur on the skin after skin injury. Mucormycosis occurs when a susceptible person comes in contact with its spores in the environment. This contact can happen at the skin (spores can enter through cuts, abrasions or wounds) or respiratory mucosa (through inhalation). The fungus is ubiquitous, and the spores are commonly found in the surrounding environment. This disease is not contagious and cannot be transferred from person to person or between people and animals.
Types of mucormycosis:
• Rhino-orbito-cerebral mucormycosis (ROCM)
• Pulmonary mucormycosis
• Gastrointestinal mucormycosis
• Cutaneous mucormycosis
• Disseminated mucormycosis
Originally, mucormycosis was described by Paltauf in 1885, as an infection from nonseptate, broad, branching hyphae typical of molds. However, the first recorded human infection with Mucorales was a case of pulmonary mucormycosis reported by Sluyter in 1847. In 1943, the syndrome of acute orbital mucormycosis characterized by uncontrolled diabetes, unilateral internal and external ophthalmoplegia, proptosis, meningoencephalitis, and rapid death was first described by Gregory. Currently India is having the second largest Covid affected population in the world. India is also the diabetes capital of the world with nearly 7.7% of adult population being diabetic. More than 6.5 Crore people in India are diabetic.
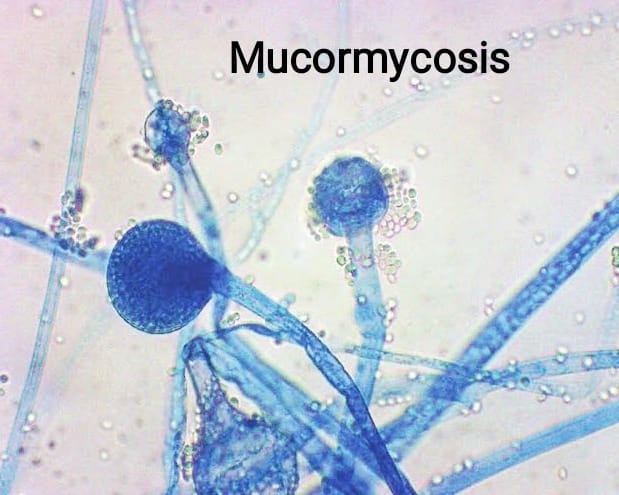
Mucormycetes, the group of different types of fungi can cause mucormycosis. The most common causative agents are Rhizopus species and Mucor species. Other causative fungi are Lichthemia, Rhizomucor, Apophysomyces, Syncephalastrum species, Cunninghamella , etc. Belonging to the scientific order Mucorales, these mucormycetes live throughout the environment.Humans acquire the infection predominantly by inhalation of sporangiospores, occasionally by ingestion of contaminated food or traumatic inoculation. They are more common in soil with decaying organic material, compost piles animal dung, and also present in the air.
Population at risk- All those who have lowered immunity are at an increased risk as this is an opportunistic infection. The list can include people who have the following-
• Post COVID-19 recovered population
• Elderly male population
• Uncontrolled hyperglycaemia with or without diabetes mellitus
• Malignancy (Eg: Leukaemias, Lymphomas, Aplastic anaemia, Thalassemia)
• Immunocompromised patients
• Organ transplant
• Stem cell transplant
• Iron overload (COVID-19, Bone-marrow transplantation, hemochromatosis, Therapy with iron chelators such as Desferrioxamine)
• Neutropenia, Monocytopenia
• Long-term corticosteroid use
• Intravenous drug abuse
• Skin injury due to surgery, burns, or wounds
• Prematurity and low birthweight (for neonatal gastrointestinal mucormycosis)
• Tuberculosis
• Patients living with Human immunodeficiency virus
• Chronic kidney disease
• Hepatitis-B and other Chronic Liver diseases
• Chronic alcoholics and smokers
• Cancer Chemotherapy
• Prolonged ICU stay
• Immunosuppressive therapy as part of COVID-19 treatment
Sign and symptoms
Signs and symptoms of mucormycosis depend on the location in the body of the infection. Infection usually begins in the mouth or nose and enters the central nervous system via the eyes.
If the fungal infection begins in the nose or sinus and extends to brain, symptoms and signs may include one-sided eye pain or headache, and may be accompanied by pain in the face, numbness, fever, loss of smell, a blocked nose or runny nose. The person may appear to have sinusitis. The face may look swollen on one side, with rapidly progressing “black lesions” across the nose or upper inside of mouth. One eye may look swollen and bulging, and vision may be blurred.
Fever, cough, chest pain, and difficulty breathing, or coughing up blood, can occur when the lungs are involved. A stomach ache, nausea, vomiting and bleeding can occur when the gastrointestinal tract is involved. Affected skin may appear as a dusky reddish tender patch with a darkening centre due to tissue death. There may be an ulcer and it can be very painful.
Invasion into the blood vessels can result in thrombosis and subsequent death of surrounding tissue due to a loss of blood supply. Widespread (disseminated) mucormycosis typically occurs in people who are already sick from other medical conditions, so it can be difficult to know which symptoms are related to mucormycosis. People with disseminated infection in the brain can develop mental status changes or coma.
Mechanism
Most people are frequently exposed to Mucorales without developing the disease.[30] Mucormycosis is generally spread by breathing in, eating food contaminated by, or getting spores of molds of the Mucorales type in an open wound. It is not transmitted between people.
The precise mechanism by which diabetics become susceptible is unclear. In vivo, a high sugar alone does not permit the growth of the fungus, but acidosis alone does. People with high sugars frequently have higher iron levels, also known to be a risk factor for developing mucormycosis. In people on deferoxamine, the iron removed is captured by siderophores on Rhizopus species, which uses the iron to grow.
Diagnosis
The finding of any of these signs should prompt immediate further testing:
Nasal Endoscopic Examination
•Black Necrotic tissue and eschar Blood tests
•CBC (Look for neutropenia / monocytopenia, Raised ESR)
•FBS, PPBS, HBA1C
•LFT, RFT with electrolytes
•HIV, HBsAg
Radiographic imaging
• X-Ray PNS (Para Nasal Sinuses) and OPG (Ortho-Pantomogram) – can be normal
• CECT of PNS and Orbit – Erosion and thinning of hard tissues, mucosal thickening of sinuses, enlargement of masticatory muscles
• Contrast MRI – Optic neuritis, intracranial involvement, CST, Infratemporal fossa involvement
• HRCT Chest - Reverse halo sign: nodule (≤3 cm)/ mass (>3 cm) or consolidation with surrounding groundglass opacity halo, central necrosis and air-crescent sign
Biopsy
Nasal cavity for ROCM, if palatal involvement then biopsy from oral cavity, Transbronchial biopsy and BAL (for Pulmonary). CT guided FNAC can be considered in some cases of Pulmonary Mucormycosis.
Histopathology
Broad ribbon-like, thin-walled, primarily aseptate or pauci septate hyphae that have irregular diameters; with non-dichotomous irregular branching and accompanying tissue necrosis and fungal angioinvasion. (GrocottMethenamine Silver GMS and Periodic Acid-Schiff PAS stains).
Direct microscopy - KOH mount (or fluorescent wet mount): an inexpensive, yet invaluable method to rapidly give a presumptive diagnosis. Mucorales are seen as broad ribbon-like, thin-walled, primarily aseptate or pauci septate hyphae that have irregular diameters; with non-dichotomous irregular branching.
Culture and sensitivity testing – Mucorales grow on any carbohydrate substrate. Colonies appear usually within 24–48 h and identification is based on colonial / microscopic morphology and growth temperature. Matrix assisted laser desorption ionization-time of flight mass spectrometry (MALDI TOF) can be used in equipped settings. The major concern about culture, however, is its low sensitivity, as it can be falsely negative in up to 50% of mucormycosis cases. Hence a combination of clinical and laboratory work up is essential to arrive at the actual diagnosis.
Molecular methods – Molecular techniques such as PCR can be used to identify this fungus directly from the infected tissues or from bronchalveolar lavage. However, these tests require invasive sampling (biopsy, bronchalveolar lavage). Recently, Mucorales DNA detection in non-invasive specimens like serum have been found to be effective for early diagnosis of mucormycosis.
Serology - There are no commercially available antigen markers to detect Mucorales. β-Dglucan test and Aspergillus galactomannan tests do not detect antigen components of the Mucorales cell wall. These two tests can help to rule out invasive aspergillosis, the most frequent differential diagnosis, or combined Aspergillus and Mucorales infections.
Few additional points on Mucor and COVID19
• Increase in ferritin level is commonly seen in COVID–19 patients. Iron overload can lead to increased susceptibility to Mucormycosis
• Prolonged use of higher end antibiotics can kill the bacterial commensals, leading to proliferation of fungal commensal such as Rhizopus or Mucor and generating a susceptible environment to cause Mucormycosis
• Excessive use of steroids can aggravate hyperglycaemia and in turn create a conducive environment for proliferation of fungi.
• Intubation, Mechanical ventilation, Chronic respiratory disease can lead to damaged epithelial and endothelial tissues – site for fungal angioinvasion
• Besides, the diffuse alveolar damage with severe inflammatory exudation, COVID-19 patients always have immunosuppression with a decrease in CD4 + T and CD8 + T cells. Severe form of COVID-19 illness is also found to reduce the level of lymphocytes as well as neutrophils. Both of which increase the chances of getting Mucormycosis infection.
Use of steroids and broad-spectrum antibiotics in COVID-19, coupled with uncontrolled hyperglycaemia has found to have increased the incidence of mucormycosis. Mucormycosis can be seen in both active COVID-19 patients and in postrecovered individuals.
Case fatality rates of mucormycosis according to previously reported data are as high as 50-70% and hence, prime importance should be laid on preventing the occurrence of this disease and eliminating all the risk factors leading to the infection in future. As per reports, prevalence of CAM is more among patient with diabetes.
Hyperglycaemia affects the immunity and also provides favourable environment for the growth of
fungi.
Primary Prevention
• Proper usage of masks (universal)
• Avoid activities that involve contact with soil or dust, such as dusting or yard work or gardening
• Hand-hygiene is a good way to avoid transferring infection from hands to the respiratory mucosa
• Proper wound care (Surgical dressing, usage of antiseptic, debridement)
• Strict glycaemic control and regular blood glucose monitoring
• Strict adherence to Anti-Diabetic medications
• Post COVID follow up and daily blood glucose monitoring in previously nondiabetics as well
• Diet and Lifestyle modifications for preventing Diabetes
• Cessation of smoking and alcohol
• Avoidance of self-medication
• Compulsory Health education to patients suffering from Covid-19 and those who have been discharged from either home isolation or facility-based treatment
• Information dissemination, Risk communication and Health education to public on early warning signs and symptoms
Secondary Prevention
• Mass chemoprophylaxis is current ly not recommended
• Currently no vaccine is available for prevention of Mucormycosis
• PNS endoscopy in post COVID-19 patients who are at increased risk of development of mucormycosis (such as uncontrolled diabetics) for twomonths
• Judicious use of antibodies/ antifungals and steroids
Early detection of mucormycosis as well as risk factors/ associated comorbidities can help prevent severe form of disease, disability, invasive treatment and death.
Treatment
The overall management of Mucormycosis should be started as early as possible. Management can involve consultation with various experts like infectious disease specialist, microbiologist, histopathologist, intensivist, pulmonologist, neurologist, ENT specialist, ophthalmologist, dentist, surgeons, and radiologists. People who are suspected of having mucormycosis should contact their nearest healthcare provider at the earliest and then seek care from the above listed specialists as per the involvement of the organ.
Basic principles of treatment
• Strict control of hyperglycaemia is vital
• Steroids are lifesaving drugs in COVID-19 patients, but abuse / misuse / untimely use must be avoided
• Judicious immunomodulating drugs
• Surgical debridement: Infected tissues are generally removed through surgical procedure at the earliest
• Monitor patients clinically, with radioimaging for response / disease progression & microbiologically
• After 3-6 weeks of amphotericin B therapy, consolidation therapy for 3-6 months
Disclaimer: The above information is for informational purposes only and is not for therapeutic purposes. Please consult a doctor or skin care professional before use.