BENIGN PROSTATIC HYPERPLASIA
The Prostate, which is part of the male reproductive system, is an exocrine gland that encloses the male urethra and its base is located at the bladder neck. A thin layer of connective tissue separates the prostate and seminal vesicles from the rectum posteriorly. There are three distinct zones found in the prostate gland. These are (a) the peripheral zone, (b) the transitional zone and (c) the central zone.
The peripheral zone, which is approximately 70% of the prostate, is the most common origin of carcinoma, chronic prostatitis, and post inflammatory atrophy.
The central zone covers 25% of the prostate gland. It is cone-shaped and is located at the base of the prostate adjacent to the seminal vesicles. The central zone also contains approximately a third of the ducts, which secrete fluid that helps to create semen. The transition zone makes up 5% volume of the gland and surrounds the urethra. The prostate gland is enclosed by a fibrous tissue layer acalled prostate capsule.
The primary function of the prostate gland, which is regulated by testosterone, is to secrete a fluid that is added together with the spermatozoa from the seminal vesicles to constitute majority of semen. This secretion is known to facilitate sperm motility and survival by providing a protective and fluid medium for their passage through the vagina for fertilisation.
The prostatic secretions are a milky white mixture of simple sugars (such as fructose and glucose), enzymes, and alkaline chemicals. The sugars secreted by the prostate function as nutrition for sperm as they pass into the female body to fertilise ova. Enzymes work to break down proteins in semen after ejaculation to free sperm cells from the viscous semen. The alkaline chemicals in prostatic secretions neutralise acidic vaginal secretions to promote the survival of sperm in the female body. Without this fluid, the sperm cells may find it difficult to reach the egg, because this weakly alkaline fluid prolongs the lifespan of the sperm by neutralising mildly acidic environment in the vaginal tract.
Benign prostatic hyperplasia Also called benign prostatic hypertrophy
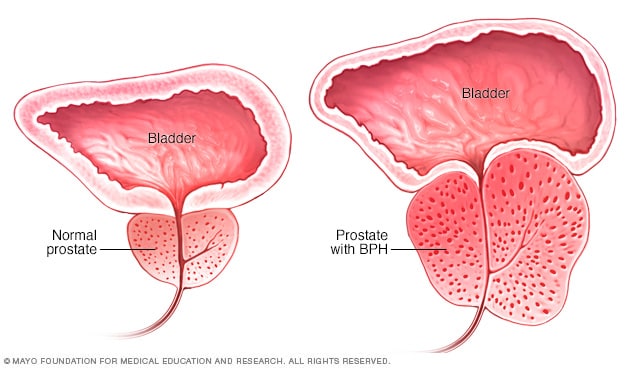
Benign prostatic hyperplasia (BPH) is enlargement of the prostate gland due to an increased number of cells (hyperplasia). Most of the growth occurs in the transition zone of the prostate. The prostate naturally gets larger as men age. Almost all men by the age of 70 will have some prostate enlargement. BPH does not increase the risk of prostate cancer.
Risk factors
Other than increasing age, there are no risk factors for BPH.
Cause
The cause of benign prostatic hyperplasia is not well understood; however, it occurs mainly in older men. Benign prostatic hyperplasia does not develop in men whose testicles were removed before puberty. For this reason, some researchers believe factors related to aging and the testicles may cause benign prostatic hyperplasia.
Throughout their lives, men produce testosterone, a male hormone, and small amounts of estrogen, a female hormone. As men age, the amount of active testosterone in their blood decreases, which leaves a higher proportion of estrogen. Scientific studies have suggested that benign prostatic hyperplasia may occur because the higher proportion of estrogen within the prostate increases the activity of substances that promote prostate cell growth.
Another theory focuses on dihydrotestosterone (DHT), a male hormone that plays a role in prostate development and growth. Some research has indicated that even with a drop in blood testosterone levels, older men continue to produce and accumulate high levels of DHT in the prostate. This accumulation of DHT may encourage prostate cells to continue to grow. Scientists have noted that men who do not produce DHT do not develop benign prostatic hyperplasia.
Signs and symptoms
In the early stages of BPH, there are no signs and symptoms. They appear when the prostate begins to squeeze the urethra and cause changes in bladder habits:
-difficulty passing urine
-frequent urination (especially at night)
-weak or slow urinary stream
-inability to empty bladder completely
-stopping or starting the uri-nary stream dribbling
-blood in the urine
Diagnosis
If the signs and symptoms of BPH are present, tests will be done to make a diagnosis. Tests may include:
-Medical history and physical examination
-digital rectal examination: Digital Rectal Examination (DRE) is a procedure where the doctor inserts his finger (the Digit) in the patient’s anus (the entrance to the Rectum) in order to feel the condition of the prostate a questionnaire to measure how severe the bladder problems are and how they affect the man’s quality of life
-Urinalysis: Urinalysis involves testing a urine sample.
PSA blood test: Blood for a PSA test is drawn. Prostate cells create a protein called PSA. Men who have prostate cancer may have a higher amount of PSA in their blood. However, a high PSA level does not necessarily indicate prostate cancer. In fact, benign prostatic hyperplasia, prostate infections, inflammation, aging, and normal fluctuations often cause high PSA levels. Much remains unknown about how to interpret a PSA blood test, the test’s ability to discriminate between cancer and prostate conditions such as benign prostatic hyperplasia, and the best course of action to take if the PSA level is high.
-Urodynamic Tests: Urodynamic tests include a variety of procedures that look at how well the bladder and urethra store and release urine. Most urodynamic tests focus on the bladder’s ability to hold urine and empty steadily and completely and may include the following:
Uroflowmetry, which measures how rapidly the bladder releases urine postvoid residual measurement, which evaluates how much urine remains in bladder after urination reduced urine flow or residual urine in the bladder, which often suggests urine blockage due to benign prostatic hyperplasia
Cystoscopy, a procedure that uses a tubelike instrument, called a cystoscope, to look inside the urethra and bladder. A urologist inserts the cystoscope through the opening at the tip of the penis and into the lower urinary tract. A urologist may use cystoscopy to look for blockage or stones in the urinary tract.
Transrectal ultrasound: Transrectal ultrasound uses a device, called a transducer, that bounces safe, painless sound waves off organs to create an image of their structure. Urologists most often use transrectal ultrasound to examine the prostate. In a transrectal ultrasound, the technician inserts a transducer slightly larger than a pen into the man’s rectum, next to the prostate. The ultrasound image shows the size of the prostate and any abnormalities, such as tumors. Transrectal ultrasound cannot reliably diagnose prostate cancer.
Imaging include
o Kidney, bladder and prostate ultrasound
o Ultrasound to determine how much urine remains in the bladder after urination (residual urine)
o Transrectal ultrasound (TRUS) guided biopsy
These tests are used to confirm the diagnosis of BPH, rule out other problems such as a urinary tract infection or prostate cancer, and check for any complications related to BPH.
Treatment:
Treatment options for BPH may include the following:
Observation
Watchful waiting (active surveillance) means watching closely for signs or symptoms of disease progression without giving any treatment. It may be used with men who have few or only mild symptoms.
Drug therapy
When the symptoms of BPH are creating trouble to person than following medicines are prescribed
5-alpha-reductase inhibitors
These drugs stop testosterone, a male sex hormone that causes male sex characteristics to develop (such as deep voice and facial hair) and stimulates the development of the male reproductive system and sexual activity from being changed into another form within the prostate called dihydrotestosterone, which is believed to cause the prostate to enlarge. They work best in men with large prostates. The medication takes several months to shrink the prostate and relieve symptoms.
The two drugs in this class are finasteride and dutasteride. Side effects include:
-decrease in sexual desire
-erectile dysfunction
-smaller amounts of semen with ejaculation
-swollen and/or tender breasts
Alpha-adrenergic blockers
These drugs relax the muscles near the prostate to relieve pressure on the urethra and allow urine to flow more easily. They do not shrink the size of the prostate.
The most common drugs are:
-terazosin
-doxazosin
-tamsulosin
-alfuzosin
Side effects include:
-dizziness
-fatigue
-headache
-low blood pressure
-retrograde ejaculation
o Semen enters the bladder during ejaculation instead of going out the urethra.
Surgery
Surgery for BPH may be used for men who have severe symptoms or are completely unable to urinate or when drug therapy has not worked.
Transurethral resection of the prostate (TURP)
TURP is the removal of prostate tissue through the urethra to reduce the size of the prostate. It is the most common surgical procedure done for BPH:
-Either general or spinal anesthesia is used.
-A special tube with a light and camera (resectoscope) is inserted through the urethra into the prostate.
-The surgeon is able to see inside the urethra, prostate and bladder.
-Excess tissue is trimmed from the prostate around the urethra.
-A catheter is placed into the bladder to drain urine.
-The catheter is removed once the urine becomes free of blood (usually after 24 hours).
Side effects of TURP include:
-bleeding
-infection
-retrograde ejaculation
-erectile dysfunction – rare
-incontinence – rare
Some men may need a second procedure (10% of men after 10 years).
Other surgeries
Other forms of surgery, many similar to TURP that may be used are:
Transurethral incision of the prostate (TUIP)
o One or 2 cuts are made in the prostate to relieve the constriction of the urethra.
o TUIP is used on smaller prostates.
Transurethral needle ablation (TUNA)
o Prostate tissue is urned away using radiofre quency waves delivered through a needle.
Transurethral electrovaporisation (TUVP)
o Prostate tissue is burned away using an electrical current.
Transurethral
microwave thermo therapy (TUMT)
o TUMT uses microwaves to destroy excess prostate tissue.
o A microwave antenna is in serted through the urethra, and the microwaves heat and damage the prostate tissue.
Holmium laser resection
o A holmium laser can be used to cut out (enucleate) or vaporise the prostate. Photoselective vaporisation of the prostate (PVP)
o A powerful green laser is used to vaporise the prostate.
o It is photoselective because the red prostate tissue selectively absorbs the green laser.
o The laser is delivered througha cystoscope, and there is minimal bleeding.
Expandable braided wire-mesh urethral stents
o Stents may be used to relieve urinary obstruction caused by BPH.
High-intensity focused ultrasound (HIFU)
o HIFU is a minimally invasive procedure that allows the surgeon to destroy prostatic tissue using high energy sound waves.
Disclaimer: The above information is for informational purposes only and is not for therapeutic purposes. Please consult a doctor or skin care professional before use.