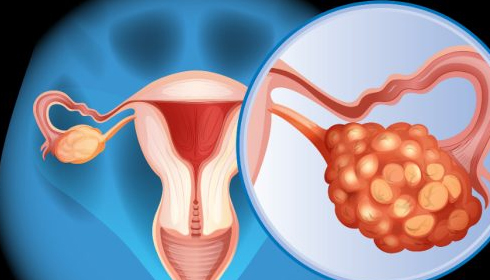
How Family Genetics Can Influence Ovarian Cancer Risk: What You Need to Know
Nearly 25% of all ovarian cancer cases are linked to family genetics, leaving many women with a difficult question: What should you do if your mother or sister is diagnosed with ovarian cancer?
The first step is understanding whether you are at high risk. According to Dr. Shaina Bruce, a gynecologic oncologist at Penn State Cancer Institute, a genetic test is key to determining if you carry the genes that could increase your risk for ovarian cancer.
If your test reveals a genetic mutation, especially on the BRCA1 or BRCA2 genes, you may face a heightened risk. BRCA1 mutations, for instance, increase the likelihood of developing ovarian cancer by 40%, while BRCA2 mutations carry a 20% higher risk. These genes also elevate the risk for other cancers like breast and prostate cancer.
For women with these mutations, preventive surgery is often recommended. "Women at increased risk for ovarian cancer are typically advised to have their fallopian tubes and ovaries removed once they are done having children," Dr. Bruce explains. However, removing ovaries early can lead to surgical menopause, which has its own health challenges, such as increased risks for heart disease, osteoporosis, and dementia due to the loss of estrogen.
Interestingly, research over the past decade has revealed that over 80% of ovarian cancers actually begin in the fallopian tubes. In response, Penn State is currently participating in a study that explores removing only the fallopian tubes in women with BRCA1 mutations while delaying ovary removal to reduce the risk of surgical menopause.
Another option for women who plan to have their "tubes tied" is to request full removal of the fallopian tubes, which can further reduce ovarian cancer risk.
Whether it’s the removal of just the fallopian tubes or both the tubes and ovaries, the procedure is minimally invasive. "It’s typically an outpatient surgery with three small incisions, and recovery usually takes a couple of weeks," Bruce said.
For those who wish to delay surgery, regular screening is an alternative. This involves transvaginal ultrasounds and blood tests to detect cancer markers. While surgery is generally recommended for BRCA1 patients between ages 35 and 40 and for BRCA2 patients between 40 and 45, screening can safely continue until they are ready for surgery.
Dr. Bruce emphasizes that preventive surgery is much less invasive compared to treatment for ovarian cancer. "Knowledge is power," she says. "If you know you have a predisposition, there’s often something that can be done about it. Preventive measures are usually far less invasive than treatment after a cancer diagnosis."
In addition to genetics, other factors that may increase the risk of ovarian cancer include hormone replacement therapy post-menopause, never having been pregnant, and conditions like endometriosis.
If you are genetically predisposed or at risk, consulting with a healthcare provider is crucial to assess your options for reducing the chances of developing ovarian cancer.