Managing Osteoporosis: The Vital Importance of Early Diagnosis, Diet, and Lifestyle
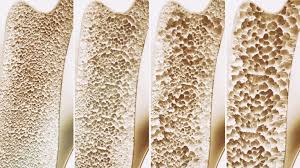
Osteoporosis, a silent and progressive bone disease, weakens bones by gradually reducing bone mineral density and mass, increasing the risk of fractures. Frequently, the condition presents no visible symptoms until a fracture occurs, often from minor incidents such as a small slip or twist.
Dr. Saurabh Chandra, a consultant in Bone, Joint Replacement, and Orthopaedics at SHALBY Sanar International Hospitals in Gurugram, stresses the importance of early screening through a Bone Mineral Density (BMD) scan. This proactive approach can catch osteoporosis early, allowing for timely interventions that may prevent more severe complications.
While osteoporosis predominantly affects older women, particularly postmenopausal women due to hormone-driven bone loss, it can affect individuals of any age or gender. Fortunately, a combination of proper diet, medication, and physical activity can slow down or even prevent further bone deterioration, offering hope and improved quality of life for those at risk.
A BMD test is a critical diagnostic tool in assessing bone health. It measures the concentration of calcium and other essential minerals, helping doctors diagnose osteoporosis, predict potential fracture risks, and monitor the effectiveness of ongoing treatments. Among the most widely used methods, a dual-energy x-ray absorptiometry (DEXA) scan is quick, painless, and non-invasive, providing a comprehensive view of bone density and overall bone strength. Central DEXA scans target the hip and spine, offering a detailed assessment, while peripheral DEXA scans may assess density in the wrist or heel but are less predictive of fracture risk.
Healthcare professionals strongly recommend osteoporosis screening for women over 65, younger women with risk factors like family history or prolonged medication use, men over 70, and anyone experiencing significant loss in height or weight. Dr. Chandra encourages patients to discuss relevant lifestyle habits, past fractures, existing medical conditions, and family history with their healthcare provider to assess individual risk accurately and outline a personalized prevention and management plan.
For those diagnosed with osteoporosis or at heightened risk, treatment typically includes dietary adjustments, medications, and lifestyle changes that target bone health. Calcium and vitamin D, for example, are foundational to bone strength, with calcium playing a direct role in building and sustaining bone tissue, and vitamin D enhancing calcium absorption. These essential nutrients are found in various foods, including dairy products, leafy greens, fortified foods, and fatty fish, while sunlight is a natural source of vitamin D. A balanced intake can significantly support bone density and help slow bone loss.
In addition to diet, lifestyle adjustments can make a profound difference. Avoiding smoking, limiting alcohol intake, maintaining a healthy weight, and engaging in regular physical activity—particularly weight-bearing and strength-training exercises—are vital for bone health. Although exercise may not dramatically increase bone mass in older adults, it improves muscle strength, balance, and coordination, reducing the risk of falls and fractures that could lead to severe complications. Medical treatments, when necessary, can range from supplements to medications that help slow bone loss and support existing bone tissue.
Prevention remains the most effective strategy against osteoporosis. A proactive approach, including regular BMD screenings, enables early diagnosis and intervention, which are essential for reducing the risk of fractures and severe complications.
By working closely with healthcare providers and following recommended diet, exercise, and lifestyle guidelines, individuals can effectively manage osteoporosis, helping to maintain strong and resilient bones and a high quality of life as they age.