Osaka University Researchers Develop New Formula for Kidney Function Assessment
In a major development, scientists from Osaka Metropolitan University's Graduate School of Medicine have developed a new formula for assessing the filtration rate of the kidney, which may change the way kidney diseases are currently diagnosed.
Regular urine tests are an important element of annual health checks because they help doctors detect early signs of kidney disease. Albumin levels in urine and glomerular filtration rate (GFR) are two important measures of kidney health. In diabetics, kidney disease frequently begins with albuminuria, which is the presence of albumin, a form of protein, in the urine.
This illness causes excessive blood filtration through the kidneys, also known as hyperfiltration, which can eventually destroy the kidneys. This process eventually leads GFR to decline, which means the kidneys are less capable of filtering waste from the blood.
However, in older people, precisely detecting excessive filtration is difficult because GFR typically falls with age. This age-related deterioration makes it difficult to establish if hyperfiltration is taking place. In response to this issue, Osaka Metropolitan University researchers created a novel method for measuring GFR that takes into account a person's age, potentially improving the identification of renal illness in older persons.
Dr. Akihiro Tsuda of Osaka Metropolitan University's Graduate School of Medicine led the study, which looked at 180 persons who were being considered as potential kidney donors. The goal was to develop a novel method for detecting hyperfiltration by altering GFR readings according to a person's age.
Their findings revealed that typical techniques of assessing GFR, which include accounting for body surface area (BSA)—a measurement based on a person's height and weight—can produce erroneous results in obese people. Specifically, the study discovered that GFR without BSA correction was higher in obese people or those with impaired glucose tolerance (pre-diabetes), whereas corrected GFR did not follow the same pattern. This shows that adjusting for body surface area may conceal early indicators of hyperfiltration in these groups.
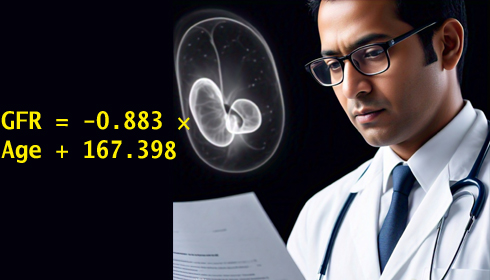
The researchers employed a mathematical model to set a new threshold for hyperfiltration and calculated GFR as GFR = -0.883 × Age + 167.398.
According to their findings, this method detects excessive filtration more accurately than the generally used GFR threshold of greater than 125 mL/min. The new formula discovered substantially more hyperfiltration than the previous method.
In persons with diabetes, hyperfiltration, or the kidneys filtering more blood than they should, is considered an early warning sign of kidney disease. If not treated, it can progress to diabetic nephropathy, a dangerous diabetes condition that can cause kidney failure. Because hyperfiltration frequently remains undetected in its early phases, precise identification is crucial for early diagnosis and treatment.
Dr. Tsuda's team's innovative technology could help clinicians detect hyperfiltration more accurately, particularly in older adults and obese patients. The new approach, which uses GFR measurements without accounting for body surface area and incorporates the natural reduction in filtration with age, provides a more exact technique to estimate kidney health.
"Since hyperfiltration is a precursor to diabetic nephropathy, we hope that using this new formula will more accurately diagnose the condition, leading to early detection and treatment," according to Dr. Tsuda.
The findings have important consequences for healthcare professionals. Current techniques of estimating GFR may ignore hyperfiltration in obese or older patients, delaying necessary therapies. Doctors can use the updated formula to better identify people at risk of developing renal disease and take preventive measures sooner.
Furthermore, the study emphasises the value of personalised medicine, which tailors medical care to particular patient characteristics such as age and body composition. This study could lead to better results for patients, particularly those with diabetes or obesity, who are more likely to have renal problems.
Additional study and validation are required before the formula may be extensively used in clinical practice. However, if applied, it could constitute a substantial improvement in nephrology, contributing to a reduction in the global burden of kidney disease.