Sharp Rise in Cervical Artery Dissection Cases Among Older, Black, and Hispanic Populations, Study Finds
A new study published in Neurology reveals a significant rise in cervical artery dissection (CeAD) cases across the United States over a 15-year period, particularly among older adults, Black, and Hispanic populations. The findings highlight the urgent need for improved awareness, early diagnosis, and targeted prevention strategies for at-risk groups.
Researchers from The Warren Alpert Medical School of Brown University, led by Dr. Liqi Shu, analyzed data spanning from 2005 to 2019 using the National Inpatient Sample, the National Readmission Database, and statewide inpatient records from New York and Florida. They identified a total of 125,102 patients hospitalized with spontaneous CeAD during this period.
The study found a dramatic increase in CeAD incidence, jumping from 10.7 to 45.6 cases per million people—an average annual percent change (AAPC) of 10.21 percent. Notably, the trend was especially pronounced in older individuals and among Black and Hispanic communities. State-level data further confirmed the national pattern, with an AAPC of 8.47 percent.
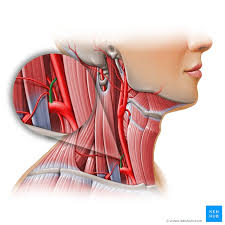
Cervical artery dissection, a leading cause of stroke in young and middle-aged adults, occurs when a tear forms in the lining of the carotid or vertebral arteries, which supply blood to the brain. This condition can lead to blood clots and ischemic strokes.
One of the most striking findings of the study was the identification of vertebral artery dissection as the sole major predictor of ischemic stroke within 90 days in patients who initially presented without a stroke. Patients with this type of dissection had a 77% higher risk of developing a stroke compared to those with other forms of CeAD.
“These results underscore the critical need for increased clinical vigilance and more robust screening strategies in vulnerable populations,” the authors noted. “Future research should prioritize identifying the most effective treatments for vertebral artery dissection to prevent stroke recurrence.”
The study also calls attention to racial and age-related health disparities, which may influence access to timely diagnosis and care. Experts suggest this data should guide public health strategies to close the gap in stroke prevention and intervention.
Some of the study's authors disclosed financial relationships with biopharmaceutical and medical device companies, though the findings offer an independent and timely perspective on an increasingly common vascular condition.