Bengaluru doctors save a preterm child weighing 1.8 kg suffering from rare liver disease
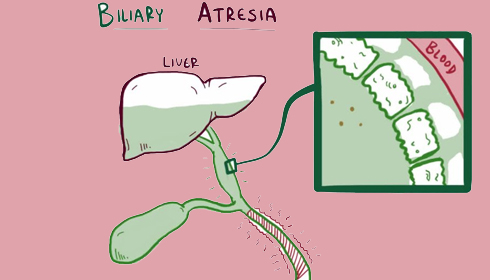
Doctors from Bangaluru’s Sakra World Hospital led by Dr Anil Kumar Pura Lingegowda, Senior Consultant and HOD-Paediatric Surgery, have saved the life of a preterm seven-day-old baby suffering from a rare liver condition known as biliary atresia, a disorder in which the bile ducts outside and inside the liver are damaged or atretic in babies.
The baby Adrija (Name changed) was born preterm at 35 weeks gestation, weighing about 1.8 kg was brought to the hospital with complaints of passing pale-coloured stools and yellowish urine.
The hospital informed that the evaluation and liver function test of Adrija suggested that she was suffering from jaundice, which is secondary to a block in the biliary system and was admitted for further investigation.
During congenital biliary atresia, bile cannot pass into the intestine and consequently collects in the liver, destroying it, leading to scarring, loss of liver tissue, and functional cirrhosis.
It may be noted that physiological jaundice commonly develops in infants and usually disappears by two weeks of age while persistent jaundice that lasts beyond two weeks needs evaluation.
Also Read:
| - Bangaluru doctors perform complex neurorehabilitation to save the life of a 36-year-old accident victim |
However, usually, infants with biliary atresia are present between the ages of three and six, but in this case, the doctors said that after investigating the baby using a specialised X-ray method called Intra-OP Cholangiogram, they found Adrija’s bile ducts were poorly developed or after which the treating doctors counselled the family on the need to undertake surgical procedures to cure her.
Adrija underwent an extended KASAI portoenterostomy after a pre-anaesthetic examination and other preoperative investigations. This is a surgical procedure to treat congenital biliary atresia in which the atretic extrahepatic bile ducts are removed and a new connection between the liver and intestine is made using a loop of her small intestine.
Following surgery, she was shifted to the NICU for post-operative monitoring where Adrija recovered steadily with supportive treatment under the guidance of Dr Shivkumar Sambargi.
Feeding was initiated at a low volume and progressed to full feeds, which she tolerated well. Then she passed yellow-coloured stools.
According to literature findings after an extended KASAI portoenterostomy, 30% of children do well after surgery, 30% do well in the initial period but later develop signs of liver failure requiring a liver transplant, and 30% do not show any improvement post-surgery and the liver deteriorates further.
Pointing out that this was the basis of their observation and concern, Dr Kumar said “In view of persistent conjugated bilirubin, Adrija was evaluated and found to have biliary atresia. KASAI portoenterostomy is the major reconstructive surgery done in newborn children for biliary atresia. The child, in this case, was premature and newborn, weighing only 1.8 kg, which was very challenging for the anaesthesia team.”
Lauding the team of Dr Shishir Chandrashekhar for managing the reconstruction surgery very well, Dr Kumar added, “It is also a technically difficult surgery to do with success. We were able to achieve that without much suffering for her.”
“We were pleased to report that Adrija responded well intraoperatively, postoperatively, and on follow-up,” he further added.
Informing that Adrija is now passing normal-coloured faeces, and her bilirubin levels have progressed to normal levels, Dr Kumar said, “Even though it is a complex disease requiring major surgery, it is possible to operate on a small infant with good results in a place where expertise and facilities are available.”