Mount Sinai Researchers Uncover Cellular Mechanism Behind Crohn's Disease
Mount Sinai researchers have found important biological pathways that could induce the emergence of inflammatory bowel disease (IBD), notably Crohn's disease, according to a recent publication in Science Immunology. The study discovered that the early depletion of gamma delta intraepithelial lymphocytes (gamma delta IELs) in the stomach could potentially trigger chronic inflammation, thereby influencing the creation of predictive biomarkers and innovative therapeutic approaches.
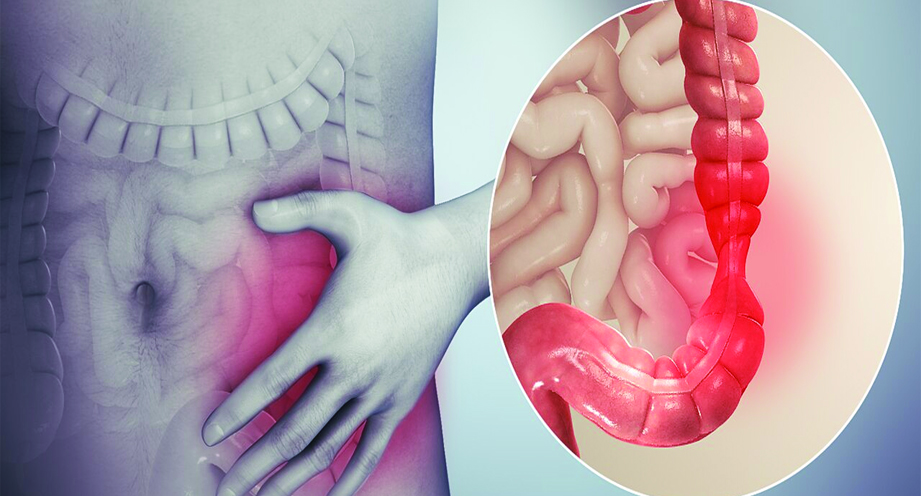
Crohn's disease, a severe form of IBD, is defined as chronic inflammation of the gastrointestinal (GI) tract, which causes stomach discomfort, diarrhoea, weight loss, anaemia, and exhaustion. The body's immune response typically includes inflammation as a defence mechanism; nevertheless, chronic inflammation can cause long-term harm to healthy tissues and organs. Gamma Delta IELs are specialised white blood cells found in the gastrointestinal system that act as a first line of defence, preventing infections and allowing tissue surveillance. Previous research had found a decrease in these cells in patients with active IBD, but their role remained unclear.
According to corresponding author Karen Edelblum, PhD, Associate Professor of Pathology, Molecular and Cell-Based Medicine at Mount Sinai, "Previous studies on patient biopsies revealed a decrease in gamma delta IELs in those with active IBD." However, it remained unclear whether the illness caused or resulted in the death of these cells. The study now shows that gamma delta IELs were lower in a mouse model of ileitis that looked like Crohn's disease weeks before any clinical or histological signs of the disease showed up. This time frame of cellular dysregulation matches data from people with IBD, suggesting that losing these regulatory cells early on may be a step towards chronic inflammation.
Researchers used a mouse model of inflammation in the lower small intestine and found that substances that cause inflammation made it harder for gamma delta IELs to talk to the cells that line the intestine.
As a result, the majority of gamma delta IELs did not survive, significantly limiting barrier surveillance. Furthermore, these cells lost their ability to inhibit other pro-inflammatory IELs, potentially resulting in uncontrolled tissue damage. According to the study, monitoring the loss of gamma-delta IELs could serve as a predictive biomarker for illness relapse or patient response to treatment, and future therapies could attempt to improve their function in order to maintain remission or avoid disease onset.
This research is vital for world health, particularly in low- and middle-income nations. LMICs frequently have inadequate resources for sophisticated diagnostic and treatment options. As a result, identifying a viable biomarker for early detection and prevention of IBD may lead to more cost-effective management techniques. Furthermore, medications developed from this research could be customised to address the unique constraints of LMIC healthcare settings, where chronic disorders like Crohn's disease exert an increasing strain on public health systems.
The Mount Sinai-led work not only sheds light on the cellular events that precede Crohn's disease; it also opens up new possibilities for early intervention and personalised therapy options. These discoveries have far-reaching consequences, with the potential to improve patient outcomes internationally while also addressing crucial healthcare concerns in resource-limited regions.